Does Medicare pay for Orgovyx? This is a crucial question for anyone considering this treatment. It’s like trying to figure out if your insurance covers that fancy new gadget—you need the details! Let’s dive into the specifics to unravel the mystery of Medicare’s coverage for Orgovyx, so you can get a clear picture of your potential out-of-pocket costs.
It’s a bit of a maze, but we’ll map it out for you.
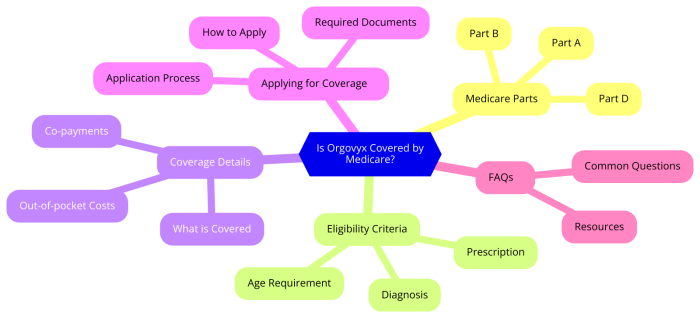
Understanding Medicare’s coverage for Orgovyx involves looking at different plan types, eligibility criteria, and potential cost-sharing responsibilities. Think of it as a puzzle; each piece, from the specific medical conditions to the financial assistance programs, contributes to the overall picture. This guide aims to break down the complexities of coverage, making it easier to understand your options.
Coverage Details
Orgovyx, a medication used in the treatment of specific cancers, presents varying coverage policies across different Medicare plans. Understanding these nuances is crucial for beneficiaries to effectively manage their healthcare costs and ensure access to this potentially life-saving treatment. This section will delve into the specifics of Orgovyx’s use, the types of coverage offered under Medicare, and important comparisons across various plans.Orgovyx is primarily prescribed for individuals diagnosed with specific advanced prostate cancers.
Its effectiveness in extending survival and improving quality of life has made it an important treatment option for many. Understanding the conditions it addresses, the coverage details, and the nuances across Medicare plans is essential for beneficiaries to make informed decisions about their care.
Use Case Summary
Orgovyx is indicated for the treatment of castration-resistant prostate cancer (CRPC) in adult patients. It is typically prescribed after other treatments have been exhausted, and its purpose is to manage the progression of the disease. The specific aim is to prolong survival and improve the patient’s overall well-being.
Specific Medical Conditions
Orgovyx is primarily prescribed for men diagnosed with advanced prostate cancer that has progressed despite initial treatments. This includes cancers resistant to standard therapies such as hormone therapy.
Medicare Coverage Types
Medicare coverage for Orgovyx varies significantly depending on the specific Medicare plan a beneficiary is enrolled in. Part D plans, for example, typically cover the medication as a prescription drug. Medicare Advantage plans, on the other hand, often combine Part A, Part B, and Part D benefits into a single package, potentially influencing Orgovyx coverage. Understanding these nuances is vital for beneficiaries to navigate the complexities of their healthcare coverage.
Comparison of Coverage Options, Does medicare pay for orgovyx
The coverage of Orgovyx under Medicare varies significantly across different plans. Factors such as formulary placement, cost-sharing, and prior authorization requirements play a critical role in determining the overall cost to the patient. Beneficiaries should thoroughly review their specific plan details to understand their potential out-of-pocket expenses.
Coverage Policies by Plan Type
| Medicare Plan Type | Typical Coverage Policy | Potential Exceptions | Additional Notes |
|---|---|---|---|
| Medicare Part D | Generally covers Orgovyx as a prescription drug. Coverage often depends on the plan’s formulary, which lists covered medications. | Certain plans may have limitations or exclusions based on prior authorization requirements or if the medication is deemed medically unnecessary. | Beneficiaries should check their specific Part D plan’s formulary and coverage details to ensure Orgovyx is included. |
| Medicare Advantage | Medicare Advantage plans often include prescription drug coverage (Part D) as part of their comprehensive benefits. Coverage depends on the specific plan’s formulary. | Similar to Part D plans, coverage may be subject to prior authorization or limitations based on medical necessity. | Medicare Advantage plans vary widely; beneficiaries must review their specific plan documents to understand the specifics of Orgovyx coverage. |
Eligibility Requirements
Medicare coverage for Orgovyx, like any prescription drug, is contingent upon specific eligibility criteria. Understanding these requirements is crucial for beneficiaries seeking coverage. This section details the necessary steps and considerations for determining eligibility.Medicare’s coverage decisions are often guided by factors like the beneficiary’s specific medical needs, the treatment plan, and the drug’s demonstrated effectiveness. Beneficiaries should consult with their healthcare providers and Medicare representatives for personalized guidance.
Medicare Beneficiary Eligibility Criteria
Medicare beneficiaries must meet specific criteria to be eligible for Orgovyx coverage. These criteria are typically evaluated based on the beneficiary’s diagnosis, treatment plan, and the drug’s approved uses. The specifics may vary depending on the individual’s circumstances.
Prior Authorization for Orgovyx
Prior authorization is a crucial step in the coverage process for Orgovyx. Medicare may require prior authorization for certain drugs, including Orgovyx, to ensure the drug is medically necessary and appropriate for the beneficiary’s specific situation. This process helps control costs and ensure the drug is used effectively. Beneficiaries should discuss the prior authorization process with their healthcare providers.
Step-by-Step Guide for Determining Eligibility
- Consult with your physician: Discuss your medical condition and treatment plan with your physician. Your physician will provide necessary documentation and recommendations regarding your need for Orgovyx.
- Obtain a prescription: Your physician will prescribe Orgovyx if deemed medically necessary.
- Contact Medicare: Contact Medicare or your Medicare plan administrator to understand the specific coverage policy for Orgovyx and the prior authorization process.
- Gather required documents: Prepare the necessary documentation to support your eligibility request. This will likely include medical records, diagnostic reports, and other relevant information.
- Submit application: Submit your eligibility request to the appropriate Medicare entity, following the instructions provided.
- Follow up on the status: Monitor the status of your application for timely resolution.
Financial Assistance Programs
Medicare may offer financial assistance programs to help cover the cost of Orgovyx. These programs may vary based on the beneficiary’s income and resource levels. Contacting Medicare or your plan administrator will provide details on available programs.
Figuring out if Medicare covers Orgovyx can be tricky, but thankfully, there are resources to help. For a delicious side dish, try out this recipe for split chicken breast on the grill recipe for split chicken breast on grill. While this recipe won’t directly answer your Medicare coverage question, it’s a great way to make a tasty meal! To get the definitive answer about Orgovyx coverage, it’s best to check with your specific Medicare plan or a healthcare professional.
Documents Needed for Verifying Eligibility
- Prescription order from a physician.
- Medical records relevant to the condition being treated.
- Diagnostic reports and test results.
- Proof of Medicare enrollment and coverage.
- Information on any other medications being taken.
Cost and Payment Information
Understanding the potential costs associated with Orgovyx is crucial for Medicare beneficiaries considering this treatment option. This section details estimated costs, the impact of Medicare Part D, and potential savings through various plan types.
Estimated Cost of Orgovyx
The estimated cost of Orgovyx varies depending on the specific prescription dosage and the pharmacy dispensing it. Pricing can fluctuate based on market factors and manufacturer discounts. It’s essential to consult with a pharmacist or healthcare provider for the most up-to-date pricing information. Typical costs range from several hundred to over a thousand dollars per month for a standard course of treatment.
Medicare coverage for Orgovyx can be tricky to figure out. While we’re not sure about specific coverage, you might find some helpful information on the different types of dog food available for allergies, such as fish-based dog food for allergies , which could be a good starting point for research on similar healthcare situations. Ultimately, checking with Medicare directly will provide the definitive answer for Orgovyx coverage.
Impact of Medicare Part D Deductibles and Out-of-Pocket Maximums
Medicare Part D plans play a significant role in covering the cost of Orgovyx. Beneficiaries will encounter a deductible amount before their coverage begins. Once this deductible is met, the plan typically covers a portion of the medication’s cost, while the beneficiary is responsible for the remaining cost-sharing. Out-of-pocket maximums, which cap the total amount a beneficiary pays for covered drugs during a plan year, also influence the overall cost.
Cost-Sharing Responsibilities
Medicare beneficiaries’ cost-sharing responsibilities for Orgovyx are dependent on their specific Part D plan. These responsibilities can include co-pays, co-insurance, and/or a percentage of the medication’s cost. Understanding these responsibilities is crucial to anticipate the out-of-pocket expenses involved. These costs vary significantly between plans and depend on factors such as the specific formulary and the patient’s benefit category within the plan.
Patient Assistance Programs
Patient assistance programs (PAPs) are available to help offset the cost of Orgovyx. These programs, often sponsored by pharmaceutical manufacturers, provide financial assistance to eligible individuals. Factors such as income and household size frequently determine eligibility for these programs. It’s essential to research available programs to determine if they might offer relief from the financial burden of Orgovyx.
Comparison of Potential Costs Across Medicare Plan Types
The table below provides a general comparison of potential cost-sharing responsibilities across various Medicare plan types for Orgovyx. Note that these are estimates and actual costs may vary depending on individual circumstances and plan specifics.
| Medicare Plan Type | Estimated Cost-Sharing (per month) | Potential Savings |
|---|---|---|
| Medicare Part D | $100 – $500 (copay/coinsurance) | Potential savings through manufacturer discounts, plan formularies, and patient assistance programs. |
| Medicare Advantage | $50 – $300 (copay/coinsurance, potentially lower than Part D) | Potential savings through lower out-of-pocket costs, bundled services, and supplemental coverage. |
Claims and Reimbursement: Does Medicare Pay For Orgovyx
Medicare’s reimbursement process for Orgovyx, like other covered medications, is designed to be efficient and transparent. Understanding this process is crucial for patients and healthcare providers to ensure timely and appropriate payment. This section details the procedures involved in submitting claims and receiving reimbursement for Orgovyx under Medicare.
Claim Submission Process
The claim submission process for Orgovyx under Medicare follows standard Medicare guidelines. Prescribers and pharmacies must adhere to specific coding and documentation requirements. Correctly completing and submitting claims is vital to ensure timely processing and reimbursement. Inaccurate or incomplete claims can lead to delays or denials. The claims process typically involves the physician’s office or the pharmacy submitting the claim to Medicare’s processing system.
Medicare Reimbursement Methodology
Medicare’s reimbursement methodology for Orgovyx, as with all covered drugs, is based on the National Drug Code (NDC) and the established payment rates for the medication. Medicare evaluates the claim, ensuring the necessary medical necessity criteria are met. Once the claim is approved, the reimbursement is processed according to Medicare’s established payment schedule. Payment amounts can vary based on factors such as the patient’s specific coverage plan.
Claim Processing Timeframe
The timeframe for Medicare claims processing for Orgovyx is typically within 30 to 45 days. However, this timeframe can vary depending on factors like claim completeness, system backlogs, or any required follow-up. Understanding the potential timeframe helps patients and healthcare providers anticipate the reimbursement process.
Claim Submission and Reimbursement Flowchart
[Note: A flowchart illustrating the claim submission process would visually depict steps such as: 1. Prescriber orders Orgovyx; 2. Pharmacy fills the prescription; 3. Pharmacy submits claim to Medicare; 4. Medicare processes claim; 5.
Medicare pays pharmacy; 6. Pharmacy reimburses provider. The flowchart would include decision points for claim denials and appeal processes.]
Appeal Process for Denied Claims
If a claim for Orgovyx is denied, Medicare provides a formal appeal process. This process allows patients and providers to contest the denial and present supporting documentation. The appeals process typically involves multiple stages, from initial reconsideration to a final decision. Appeals should be filed within specific timeframes to maintain eligibility for review. Thorough documentation and justification for the claim are crucial during the appeal process.
Important Considerations
Understanding the potential benefits and risks associated with Orgovyx is crucial for informed decision-making. This section provides details on potential side effects, resources for further information, and steps to clarify Medicare coverage. Thorough consideration of these factors will help patients and their healthcare providers navigate the treatment process effectively.
Potential Side Effects and Adverse Reactions
Orgovyx, like other medications, may cause adverse reactions in some individuals. Common side effects may include fatigue, nausea, vomiting, diarrhea, and changes in appetite. Less common but potentially serious side effects could include liver problems, skin reactions, or changes in blood counts. It is essential to report any unusual symptoms to a healthcare provider immediately. The specific side effects and their severity can vary based on individual factors, such as age, pre-existing conditions, and other medications being taken.
Close monitoring by a healthcare professional is critical during treatment.
Finding Additional Information about Orgovyx Coverage
Various resources can provide valuable information about Orgovyx coverage under Medicare. Patients should consult their healthcare providers, Medicare’s official website, and pharmaceutical information websites for accurate and up-to-date details. Understanding the specific coverage criteria and potential out-of-pocket costs associated with Orgovyx is crucial for effective planning.
Reputable Resources for Further Research
Several reputable sources offer detailed information about Orgovyx and its associated coverage under Medicare. These include the official Medicare website, the drug manufacturer’s website (if applicable), and reliable healthcare professional organizations. These sources can provide specific details about coverage, potential side effects, and dosage information.
Steps to Take When Seeking Clarification on Orgovyx Coverage
Clarifying Orgovyx coverage under Medicare can be achieved through several steps. First, contact your healthcare provider’s office to discuss your specific situation and potential coverage. Secondly, review the official Medicare website for detailed information about coverage criteria. Thirdly, consider contacting a Medicare specialist for personalized guidance. Understanding the specific details of your plan is crucial for determining coverage and potential out-of-pocket costs.
Frequently Asked Questions (FAQ) about Orgovyx Coverage under Medicare
This section addresses common questions about Orgovyx coverage under Medicare.
- What is the typical cost of Orgovyx under Medicare? The cost of Orgovyx can vary depending on individual circumstances and Medicare plan specifics. It is essential to consult with a healthcare provider and Medicare representatives to understand the potential out-of-pocket costs associated with the medication.
- Does Medicare Part D cover Orgovyx? Medicare Part D plans may or may not cover Orgovyx. Detailed coverage depends on the specific plan and its formulary. Review your plan documents carefully for specific details.
- How can I find out if my specific Medicare plan covers Orgovyx? Review your Summary of Benefits and Coverage (SBC) document, or contact your plan directly for specific coverage information. Contacting a Medicare specialist or healthcare provider can also be helpful in determining coverage.
- What are the steps I should take if my Medicare plan doesn’t cover Orgovyx? If your plan does not cover Orgovyx, explore options such as contacting the manufacturer or exploring alternative treatment options with your healthcare provider. Discuss your situation with a healthcare provider to understand available options.
Epilogue
So, does Medicare pay for Orgovyx? The answer, as you’ve seen, isn’t a simple yes or no. It depends on your specific Medicare plan, eligibility, and the circumstances surrounding your need for the treatment. This guide provides a comprehensive overview, but remember to consult with your doctor and insurance provider for personalized advice. Hopefully, this information helps you navigate the complexities of Orgovyx coverage under Medicare.
Quick FAQs
Does Medicare cover all types of cancer treatments?
No, Medicare coverage varies greatly depending on the specific treatment and the plan you have. Some treatments are covered, while others may require more investigation.
What if my Orgovyx costs exceed my out-of-pocket maximum?
Once you’ve hit your out-of-pocket maximum, Medicare generally covers the remaining costs of Orgovyx.
What is prior authorization, and how does it affect Orgovyx coverage?
Prior authorization is a process where your doctor needs to request permission from your insurance company to cover a particular treatment. This varies by plan, so check with your plan.
How can I find out more about potential patient assistance programs for Orgovyx?
The manufacturer of Orgovyx may have programs that can help reduce the financial burden. You can usually find this information on the manufacturer’s website or through your doctor.
